You're not a resident. You're a student!
💬 comments
If you want to be a resident, go to medical school first and match into a residency program.

We recently stumbled across this ludicrous video on TikTok by @annajrrna, a.k.a. Anna Jobe, BSN. If you can't be bothered to waste 86 seconds of your life watching the video and developing brain cancer afterward, feel free to read the text transcription instead:
Why would I or why should I be paid as a third-year nurse anesthesia resident? First and foremost, because the majority of third-year nurse anesthesia residents are used in the numbers as staff. Meaning that we run rooms, we provide anesthesia, we pre-op, we consent patients for procedures. Meaning we generate a lot of revenue for hospitals. That's why we should be paid. Also, fun fact, back in the day, nurse anesthesia residents were paid. There's not currently Medicare funding for nurse anesthesia residents. This is one of the things that I hope to see change over the next 10 years in the U.S. So the average anesthesia provider in the United States is over the age of 50. We have an aging workforce. We have an aging U.S. population. We have a very sick U.S. population. The need for anesthesia services is incredibly on the rise. It takes 10 years to train a CRNA. It takes 12 years to train a physician anesthesiologist. So replacing anesthesia providers is a process that takes a long time. CRNAs provide over 50% of the anesthesia in the U.S. So I hope to see, as we bargain and negotiate for better working conditions for all anesthesia trainees, I hope that nurse anesthesia residents are paid in the next 10 years Because we have a recruitment issue, we have a retainment issue and we have a retirement issue. We need more anesthesia professionals. We need more CRNAs, specifically, because we're the most cost-effective way of providing anesthesia care in the U.S. So yeah, absolutely, I think nurse anesthesia residents should be paid throughout their training. So I hope to see that change over the next 10 years as we work on this massive workforce shortage that we have.
What the fuck is an "RRNA" even? When we Googled it, the first result we got was the Wikipedia page for ribosomal RNA. Ah, that brought us some good flashbacks (nightmares?) to our college and medical school biochemistry courses. Apparently, the highly questionable use of the non-standard term "nurse anesthesia resident" is something being actively propagated as of August 2023 by the militant organization known as the American Academy of "Nurse Anesthesiology", which was previously known as the American Association of Nurse Anesthetists. How can you call a graduate-level program, with no practice requirement for post-graduate training, a "residency"? You want to call yourself a resident? Then go to medical school first, pass a series of USMLE/COMLEX exams (with satisfactory scores, of course), complete your 2+ years of clinical rotations, and match into a real fucking residency program. The takeaway from this? Everybody wants to be a doctor, but no one (except physicians and those who aspire to be one) wants to go to medical school and lift some heavy-ass textbooks.
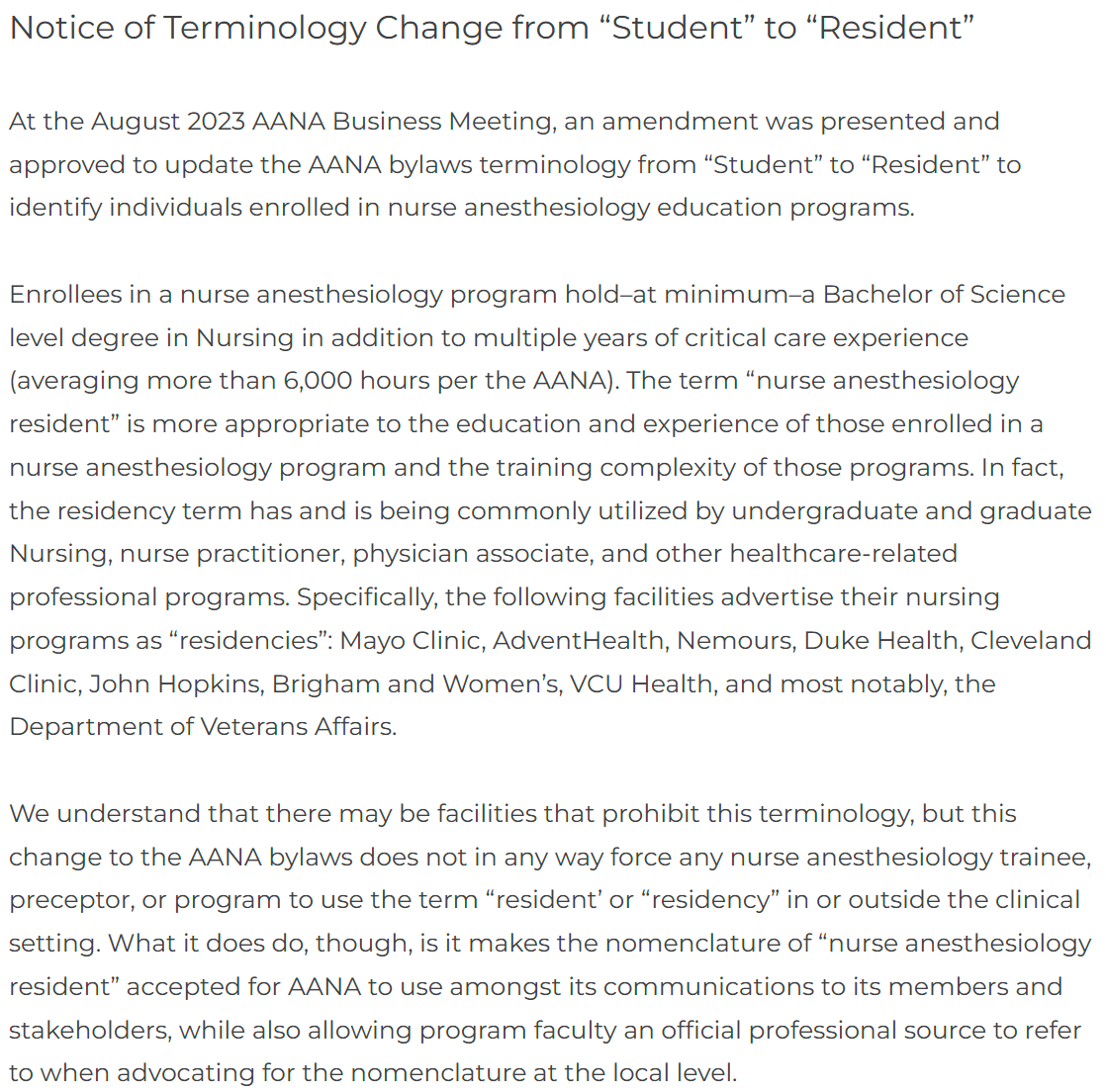
Note the AANA's not-so-subtle dig against physicians here - "In fact, the residency term has and is being commonly utilized by undergraduate and graduate Nursing, nurse practitioner, physician associate, and other healthcare-related professional programs." Other healthcare-related professional programs, like the OG ACGME-accredited residency programs for physicians? It's also worth pointing out that the AANA's claim that CRNA students hold, at minimum, "multiple years of critical care nursing experience", is demonstrably false. As with every other low-quality commodity these days, you can even get your CRNA degree online now. Check out THE Ohio State University's program, which claims to be fully online except for "intermittent" skills weeks and "intermittent" simulation days. Of course, this program only requires a minimum of one year of critical nursing experience to be considered for admission. Yeah, no thanks, why don't we stick with the board-eligible/board-certified anesthesiologist who honed their craft in person at a brick-and-mortar residency program?

Nomenclature abuse aside, there's just a couple of glaring problems with Anna the nurse anesthetist resident student's fucking insane logic here. Since when did we pay students to do the bare fucking minimum of attending school and showing up for clinical rotations? Hot damn, we're sure every medical student in the United States would love to be paid for enduring the USMLE instead of paying a king's ransom to even take it, let alone having to take out tens, if not hundreds of thousands of dollars in student loans for the rest of medical school. No wonder why Medicare doesn't fund "nurse anesthesia residents" - because you're not a fucking resident, any more than a student nurse or medical student is. We also find Anna the nurse anesthesia resident student's claim that third-year CRNA students are used as staff by running rooms, providing anesthesia, doing pre-ops, and consenting patients for procedures highly dubious. Surely hospitals and surgery centers aren't letting midlevel students doing these things without supervision?
While Anna the nurse anesthesia resident student does make some good points about the shortage of anesthesia professionals and an increasingly sick patient population, it's absolutely laughable that she brings up cost-effectiveness as an argument. As discussed above, how does it make any fucking sense to exacerbate the problem by paying students in midlevel school...while they're still in school? And it's not like CRNAs are eating ramen every day - their average salary is north of $212,000, which rivals or even exceeds that of physicians in primary care fields, particularly in academia. If anything, CRNAs should be paid less than they currently are, based on their vast differences in knowledge, training, and experience compared to a board-certified anesthesiologist. There's a reason why a physician is the big cheese of the anesthesia care team.
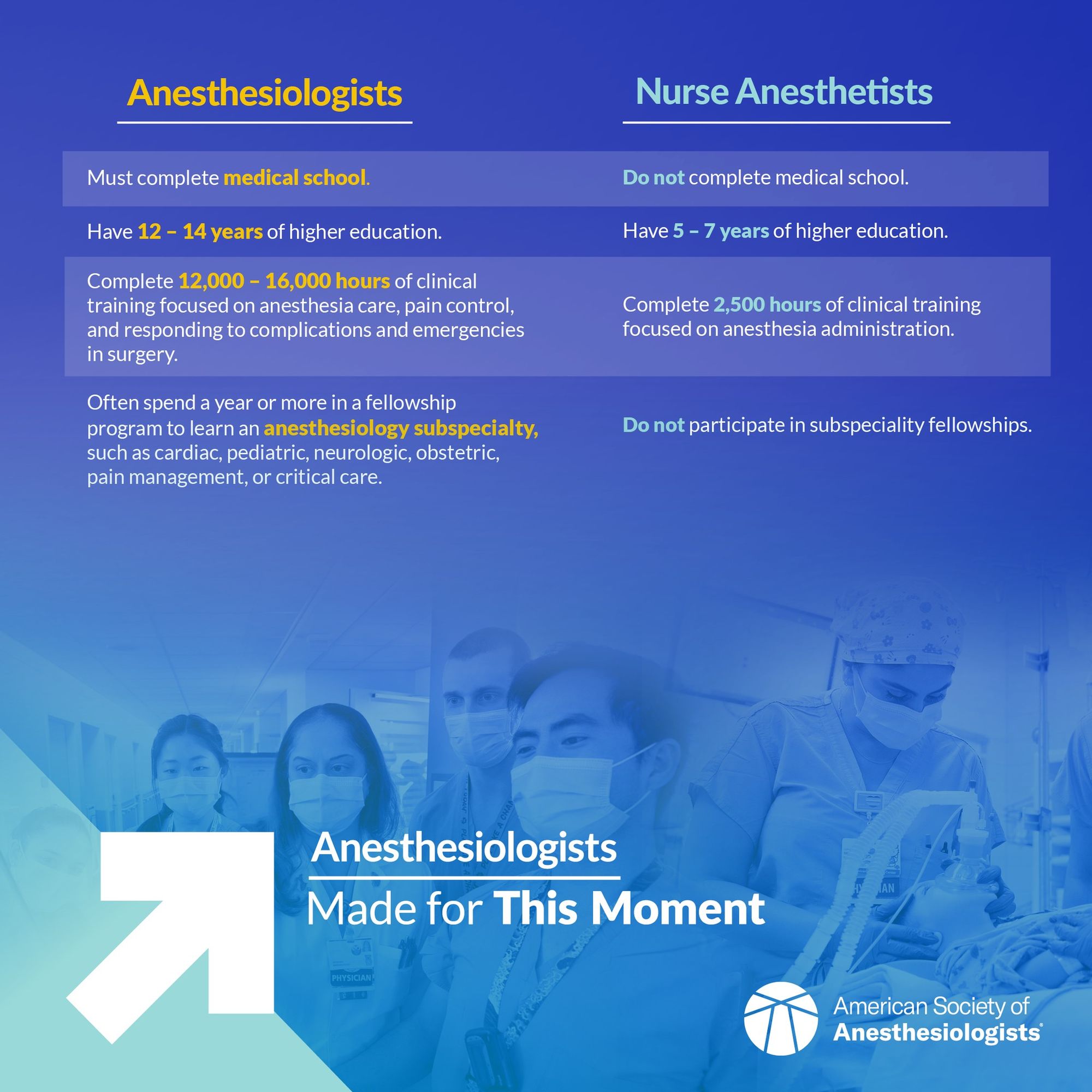
Anna the nurse anesthesia resident student claims that it takes 10 years to train a CRNA, which is demonstrably false - the typical requirement consists of 4 years to obtain a BSN degree, 3 years of CRNA school, and, as we discussed earlier, a minimum of only 1 year of critical care nursing experience in between. It certainly takes much longer to become a board-certified anesthesiologist: 4 years to obtain a bachelor's degree (traditionally in the sciences), 4 years of medical school, and 4 years of anesthesiology residency, possibly followed by 1+ years of fellowship.

Moreover, research unsurprisingly shows that patient morbidity and mortality directly increases with increased anesthesiologist staffing ratios. We take it that most hospitals would agree that racking up lawsuits and having to pay out malpractice settlements isn't a good look. But midlevel CRNAs aren't going to be disappearing anytime soon, unfortunately. Clearly, the best solution in the name of patient safety is to train more physician anesthesiologists to enable more direct supervision of CRNAs, instead of allowing these midlevels to run amok by granting them independent practice rights or acting as substitutes for physicians.

