Why midlevel supervision is an occupational hazard for physicians: the continued saga of Sarah Erny, DNP
💬 comments
As evidenced by the case of California NP Sarah Erny, midlevels are a threat to the health of their patients as well as the license and reputation of their supervising physicians.


Remember the name Sarah Erny? If you don’t here’s a quick refresher – she’s a nurse practitioner in California who gained notoriety after being fined almost $20,000 for unlawfully calling herself a “doctor” and advertising herself as such to the general public. While Ms. Erny does have a “doctorate” degree in nursing practice – the DNP – she is certainly not a physician. Despite the fact that the educational caliber and academic rigor of the DNP degree is a laughingstock when compared to that of the MD or DO degree held by physicians, that didn’t stop three more nurse practitioners from being butthurt enough to sue the state of California for the right to be called “Doctor”.

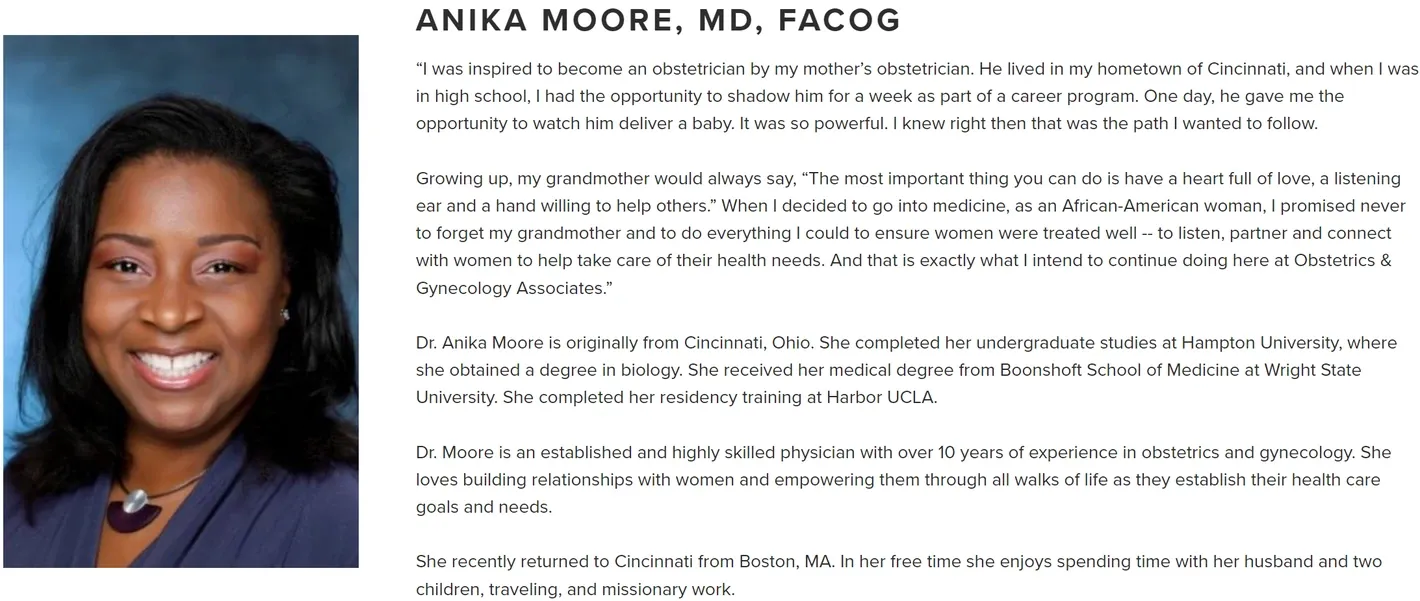
Well, the story doesn’t end there. In January of 2024, Ms. Erny’s supervising physician (i.e. an actual doctor), OB/GYN specialist Anika Moore, MD, was also fined to the tune of $25,000 by the San Luis Obispo County District Attorney for her inadequate and improper supervision of Ms. Erny. Although Dr. Moore did not admit liability as part of the final judgment, the complaint brought against her by the DA contains some damning and disturbing details about her relationship with NP Erny.

- The Collaboration Agreement was prepared by Nurse Practitioner Sarah Erny. Defendant, after receiving the Collaborative Agreement, skimmed, signed, and returned the document to Ms. Erny. Defendant, having moved to Massachusetts in 2016 to practice medicine, spent little time investigating and evaluating the circumstances in which Ms. Erny would be providing medical services under the Collaboration Agreement.
- Defendant spent no time developing the protocols within the Collaboration Agreement before her supervision of Ms. Erny began, or at any time during the approximate two years the Collaboration Agreement was in effect.
- The Collaboration Agreement included a protocol for Ms. Erny’s prescription of medications to patients, including a protocol for prescribing Schedule III through V controlled substances. However, the Collaboration Agreement did not specifically identify the permitted Controlled Substance medications that Ms. Erny could prescribe to patients.
- Defendant was unaware that Ms. Erny was prescribing controlled substance medications to patients, including the prescription of testosterone, a Schedule III medication, to both female and male patients.
- Defendant was unaware that Ms. Erny opened an independent practice as a nurse practitioner called Holistic Women’s Health near Pismo, California.
- Nor did Defendant review any physical medical records prepared by Ms. Erny.
- Defendant advised Ms. Erny that she was terminating their collaborative/supervisory business relationship on March 19, 2021, with an effective date no later than October 1, 2021.
...
- Defendant MOORE violated Business and Professions Code sections 2725 and 2836.1 and California Code of Regulations, Title 16, section 1474, by (1) failing to participate in the development of the standardized protocols with Ms. Erny in the Collaboration Agreement; (2) failing to participate in an annual review the protocols or specifically identify the controlled substances that Ms. Erny could prescribe, including testosterone, a Schedule III controlled substance; and (3) failing to perform any periodic evaluation of Ms. Erny’s performance and skills.
- Defendant has engaged in unfair business acts and practices in her cavalier attitude as to her duties and responsibilities under the Collaboration Agreement and California Law. A majority of Defendant’s supervision was limited to responding to text messages and telephone calls by Ms. Erny. Defendant was unaware of the extensive scope of Ms. Erny’s patients, including lacking any knowledge of Ms. Erny’s excessive prescribing of Schedule III anabolic steroids, treatment of male patients that Defendant had no experience as an OBGYN, and how often Ms. Erny was seeing patients, and that her clinical environment was an independent medical office. Defendant contends she had conversations with Ms. Erny regarding patient care, but failed to record any patient names and is unaware of the number of reviews she performed as a function of the patients cared for by Ms. Erny.
While one could easily argue that Dr. Moore failed to read the fine print of the collaboration agreement offered to her by NP Erny and just did a damn poor job of remotely supervising a midlevel 3,000 miles away in California while she herself lived in Massachusetts, we can easily appreciate from this case that even the most well-meaning of physicians are basically starting the timer ticking on a big fat bomb capable of destroying their professional reputation, medical licensure, and career when they agree (or are forced to by their employer) to supervise a midlevel provider such as a nurse practitioner or midlevel. How closely do you need to supervise your midlevel before they inevitably fuck up? Pretty damn close, it seems. In this particular case, NP Erny was able to prescribe excessive amounts of testosterone, a schedule III controlled substance, to both female and male patients without Dr. Moore’s knowledge. Hell, NP Erny was able to open up her own goddamn fucking independent practice without poor Dr. Moore ever being the wiser. That’s some quality supervision right there! But the million-dollar question is, was Dr. Moore ever aware that Ms. Erny was representing herself as a medical doctor to the general public?
With their limited knowledge, training, experience that amounts to little more than a nursing degree followed by a diploma mill degree and a few hundred “clinical hours” that may be nothing more than shadowing, and questionable morals and ethics, it should be pretty obvious by now to every physician out there that renting your hard-earned medical license out to a midlevel nurse practitioner for “supervision” or “collaboration” in order to make a quick buck is a serious occupational hazard. Are you staffing every one of your midlevel’s patients, like you would with a resident physician? Are you even physically on site often enough to know what exactly your midlevel is doing (or not doing)? Do you know what exactly your midlevel is prescribing to patients, potentially under your name? What kinds of sketchy compounded medications are they administering to patients, and what kinds of equally sketchy compounding pharmacies are they getting them from? If you review 10% of your midlevel’s charts for quality assurance, how can you be sure about the other 90%? What kinds of stupid questions are they not asking you and instead posting online in their stupid little NP Facebook groups?
And as evidenced by this and many other cases, guess who’s ultimately getting sued, fined, and dragged through the court of public opinion when your midlevel fucks up, even if you were never there and had no idea what went down? Indeed, supervising midlevels is kind of like working at Chernobyl in the 1980s. Everything is fine until it isn’t - one day, everything will blow up in your face and you’re left to deal with the radioactive fallout for years to come.

