Nurse practitioner's stroke of genius: it's just vertigo!
💬 comments
Why give TPA when you can give Antivert instead?

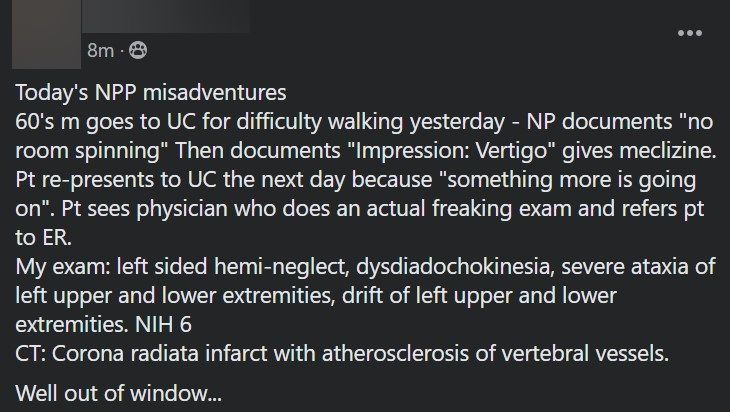
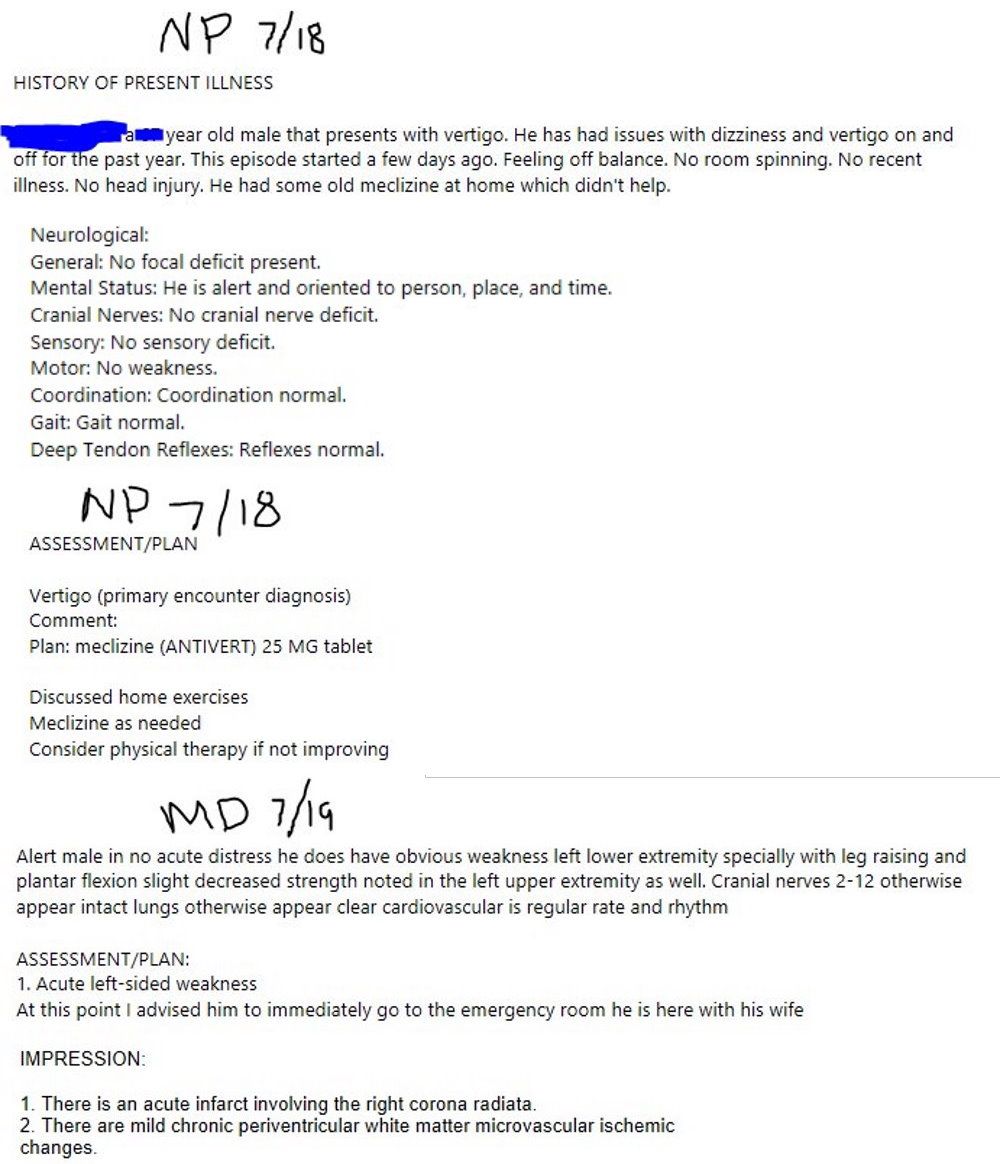
While the average layperson (and nurse practitioners, apparently) may not put too much though about what exactly it means to be dizzy, by the end of medical school most medical students are astute enough to ask patients complaining of dizziness what exactly they mean by "dizzy". Do they feel like the room is spinning around them (or vice versa)? Or do they just feel lightheaded? In a similar vein, any astute physician (particularly an emergency medicine physician or neurologist) would become immediately concerned about a patient, especially an older one, who complains acutely of being "off balance" and having difficulty walking, i.e. ataxia. Specifically, a physician who is paying even an iota of attention would immediately notice the obvious contradiction of diagnosing a patient who feels off balance, yet does not endorse room spinning, with vertigo. If it isn't already glaringly obvious by now, the concern is for acute cerebrovascular accident / stroke, specifically a posterior cerebellar stroke (although a corona radiata infarct could certainly cause ataxia as well due to hemiplegia). Unless you're a nurse practitioner, that is. Then it's just vertigo.
It is highly questionable whether the nurse practitioner at the urgent care even performed a proper physical exam. How exactly does someone who later presented with acute left-sided weakness and a NIH Stroke Score of 6 have "no focal deficit present" and "no [motor] weakness"? How could someone who complains of difficulty walking and being off-balance, noted to have severe ataxia, hemineglect, and extremity drift be documented as having a "normal gait"? The nurse practitioner's stone-cold normal physical exam, as documented, defies belief. Even if we are so generous as to give the midlevel NP the benefit of the doubt that none of these symptoms were present at the time of their exam, it's hard to see how the NP's decision to slap on a diagnosis of vertigo (while simultaneously documenting that the patient did not complain of the room spinning), prescribe some Antivert, and suggest that the patient consider physical therapy if not improving, without even entertaining the possibility of stroke or sending the patient directly to the emergency department, is even remotely medicolegally justifiable. Boy, the patient's future malpractice attorney will sure have their work cut out for them! And thanks to a couple of clues left by the anonymous birdie who originally shared this story, we even have a good idea of who the guilty nurse practitioner might be!
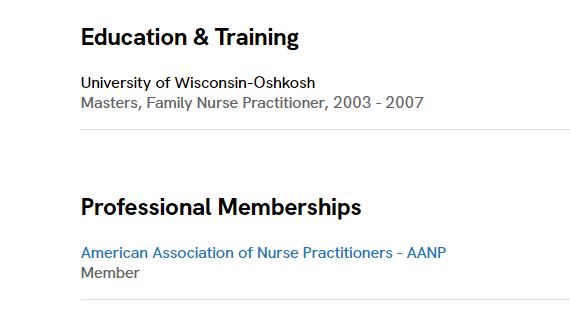
While we can only speculate on this poor patient's prognosis, one thing is for sure: time is brain. Due to their delayed presentation, this patient was not a candidate for acute ischemic stroke intervention, i.e. TPA (tissue plasminogen activator, or colloquially, "clot buster"). For our less medically-minded readers, the standard of care for patients who present to the hospital / emergency department with acute ischemic stroke, i.e. stroke presumed to be due to insufficient blood flow, e.g. from a blood clot (as opposed to a much less common hemorrhagic stroke) within 4.5 hours of symptom onset is to administer TPA, as long as no contraindications exist (such as history of recent stroke, excessive hypertension, being anticoagulated, etc.) While we can't say for sure that the patient would have been a TPA candidate, certainly the delayed recognition caused by the NP's misdiagnosis doesn't help matters. Needless to say, and without belaboring the point, the principles of stroke diagnosis and management are complicated, and a midlevel nurse practitioner who went to online school and completed a few hundred hours of shadowing (probably not in neurology or the emergency department) shouldn't be allowed anywhere near a stroke patient with a 10-foot reflex hammer. Well, at least this braindead nurse practitioner got one thing right - the patient will almost certainly be needing some physical therapy after their stroke!