Hanging in the balance: When a Facebook consult becomes a matter of life and death
💬 comments
No big deal, just send the kid home with a popsicle and call it a day. It's not like anything bad could happen.
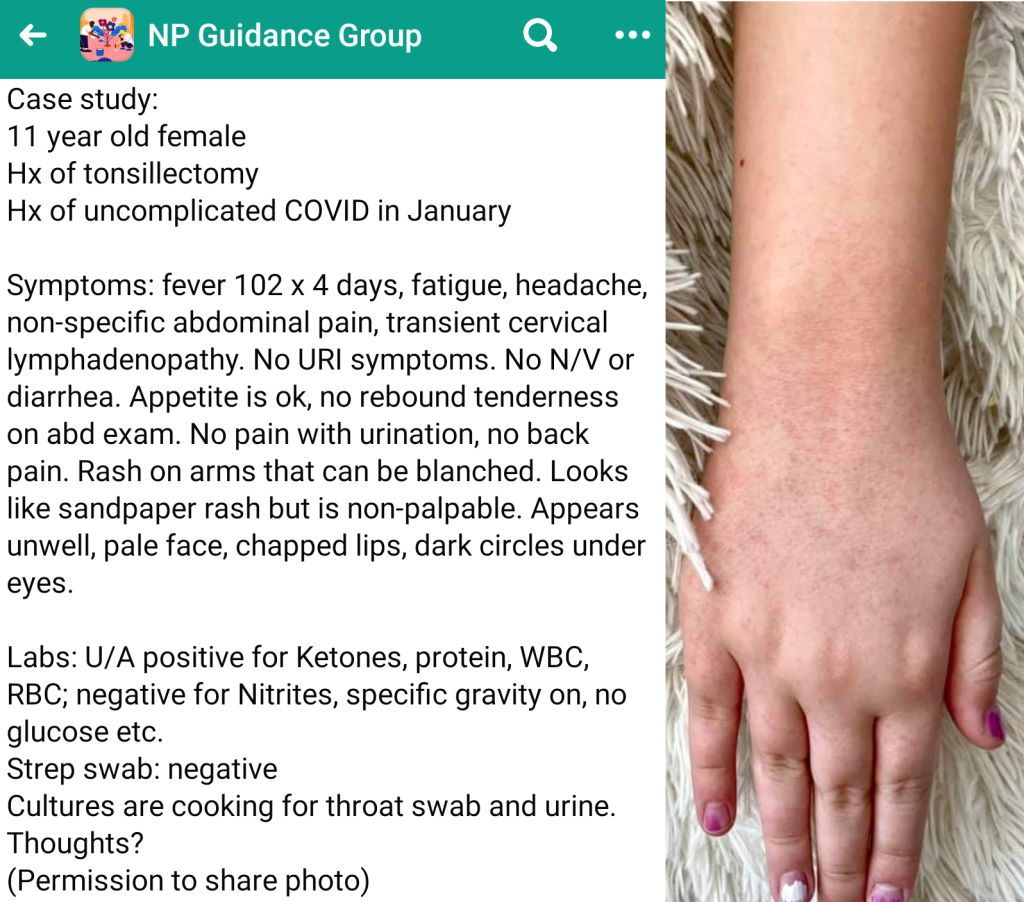
Unless they've been living under a rock, by now virtually all physicians (especially emergency physicians and pediatricians) have heard of the major post-COVID-19 sequelae that can affect children, particularly severe, life-threatening multi-system syndromes like Multisystem Inflammatory Syndrome in Children (MIS-C). I need not belabor the finer details of MIS-C for my fellow physicians reading this, but suffice it to say that many of the symptoms described with MIS-C overlap with the case presentation for Kawasaki disease, which hopefully any clinician allowed near children should be able to quickly recognize. Hell, if you're describing a kid with multiple days of fever, a sandpaper rash, chapped lips, multiple abnormalities on urinalysis including proteinuria, and looking unwell, the diagnosis is just about fucking staring you in the face. Needless to say, the standard of care for conditions like MIS-C and Kawasaki disease is at a tertiary care center with a pediatric ICU. Why the hell are you wasting time diddling around on Facebook trying to solicit medical advice for a patient presenting with symptoms consistent with an emergent, life-threatening illness, when you should be running to the phone to call EMS to have the patient transported to the nearest emergency department? Thankfully, the commenters in the peanut gallery were immediately able to rub a few brain cells together and suggest exactly that.
"Hadn't considered that?" WTF? Thankfully, NP Stefanie decided to prudently heed this advice at 4:53 PM, 14 minutes after the original post a 4:39 PM:
As a thought experiment, let's consider what might happen if no one had responded to the post. Would this midlevel still send the patient to the ER immediately? Would they provide false reassurances to the mother and send the patient home, where they might suffer permanent, life-altering sequelae or even death from complications such as coronary artery aneurysms, respiratory failure, renal failure, cytokine storm, and strokes? I sincerely hope that the patient in question here has a good outcome and recovers fully. If not, I sure wouldn't want to be around when the medical malpractice lawsuit is inevitably filed.
This is not a case study
On a related note, I'd like to also comment on the seemingly new fad/trend of midlevels in these sorts of groups trying to (poorly) disguise real-time/live patient consults/requests for medical advice as a "Case Study" in an attempt to avoid liability. This is not only a gross abuse of the concept of what a case study is, especially in a medical context, but also a terribly unethical attempt at trying to disguise a live, real-world patient case as some sort of past hypothetical situation where faulty medication decision-making doesn't have real-world consequences.