Copious vaginal discharge
💬 comments
How exactly can you work at an urgent care without ever encountering a patient with vaginal discharge?
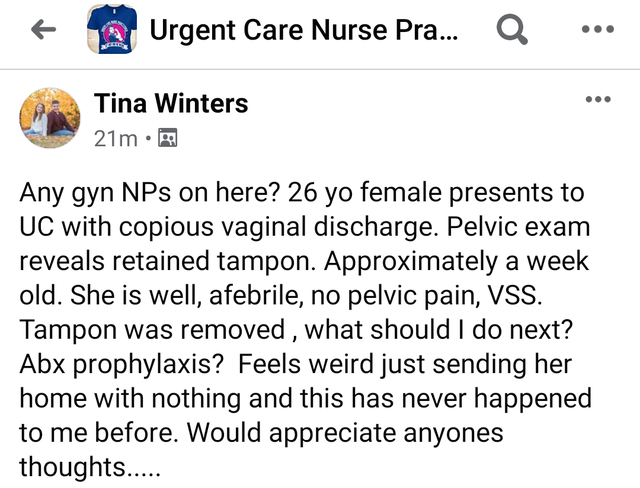
Good fucking God, on a facepalm scale from 0-10 this one is a solid 11. "What should I do next?" "Feels weird just sending her home with nothing?" "This has never happened to me before"? It is plainly evident from this Facebook post that this NP by the name of Tina Winters doesn't appear to have the slightest clue what might be going on or what a basic differential diagnosis for (copious!) vaginal discharge might be, especially in the context of a retained tampon/foreign body. And then there's all the other potential problems to worry about, like sexually transmitted infections, a yeast infection, pelvic inflammatory disease, etc. I guess we can take some solace in the fact that the patient is supposedly afebrile and hemodynamically stable, and therefore not likely to die quickly from untreated toxic shock syndrome? It certainly wouldn't be the first time a midlevel failed epically by sending a septic patient home, resulting in the patient's death! And why not ask an obstetrician/gynecologist, or even the local ED, instead of asking the Facebook peanut gallery? Did she leave the patient in the exam room, open up Facebook to post this, and then run back to the patient after someone answered? But the biggest question of all is, how in the fuck do you work at an urgent care for 1 year and 5 months without ever encountering a case of vaginal discharge? Is that even possible? Can pigs fly? Do women in New Hampshire not have vaginal discharge, ever? I guess the New England winters must, uh, really have a drying effect.
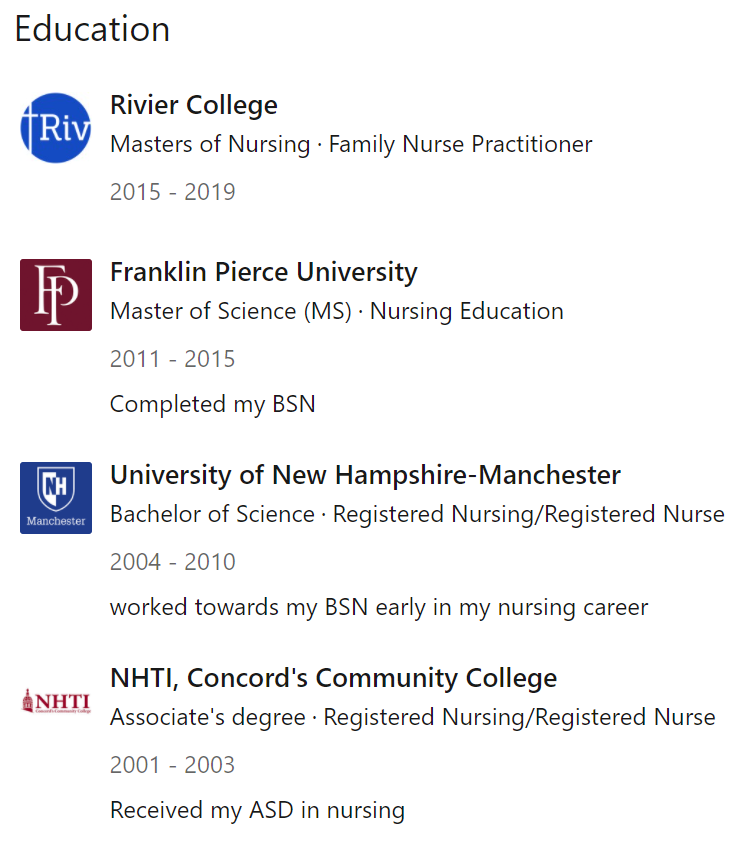
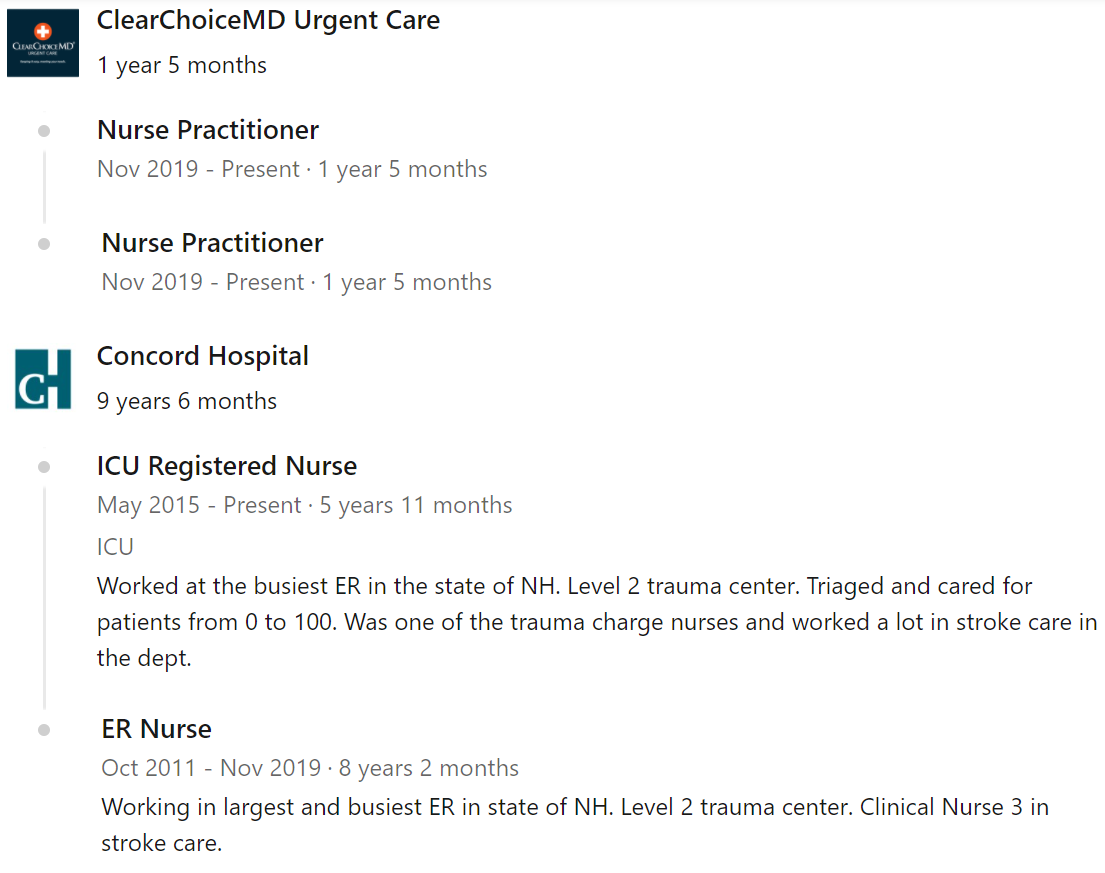
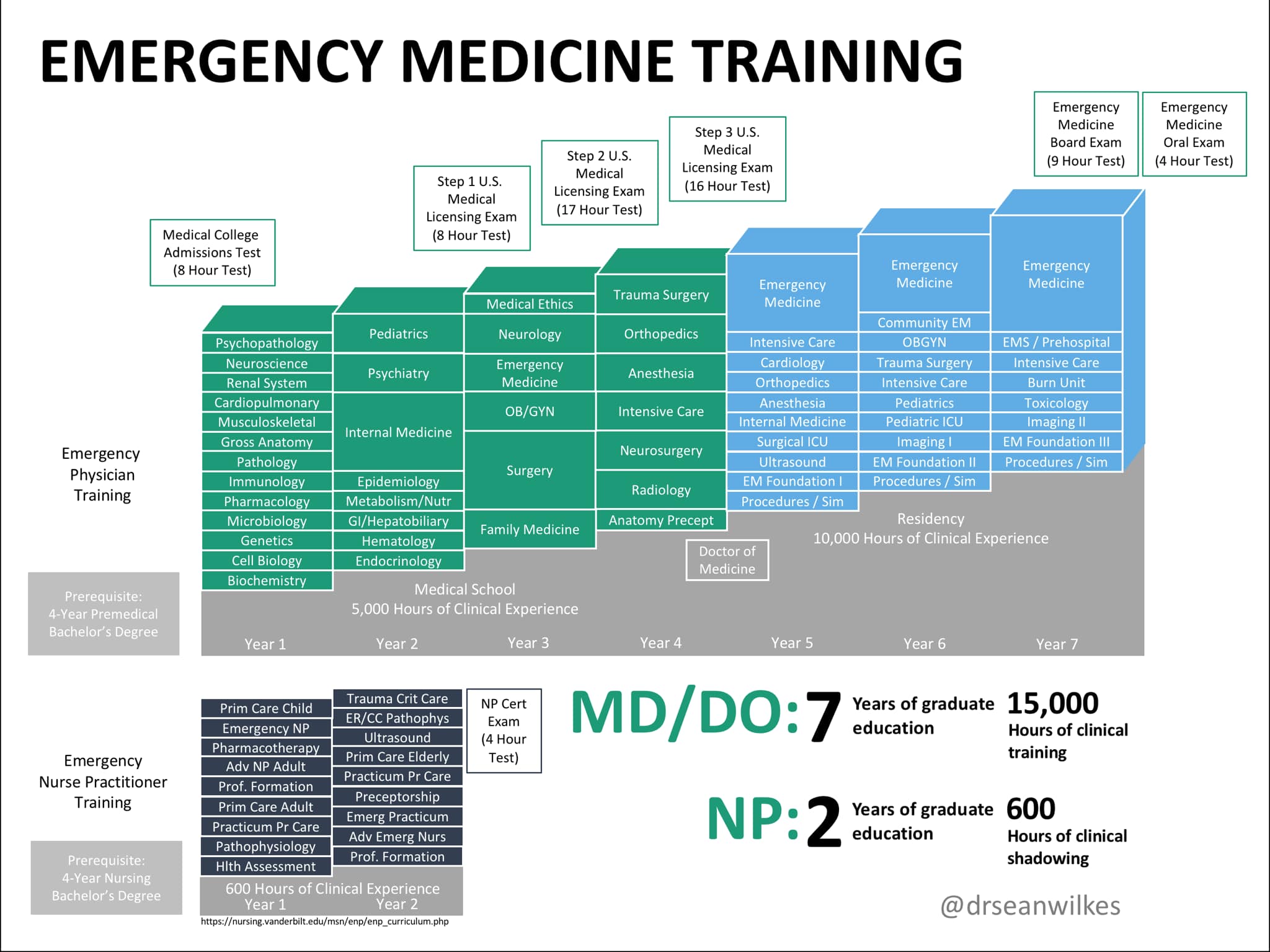
This is also a great opportunity to discuss the fundamental shortcomings of nurse practitioner education as it exists today. This particular NP has a Family Nurse Practitioner degree (courtesy of yet another online program, of course), which, arguably is a poor fit for urgent care, where hidden and potentially fatal time bombs may hide in seemingly well patients. There exists an "Emergency NP" post-master's certification which can be gained after a couple of semesters online, a few hundred clinical hours in an ED, and a 150-question AANPCB-sponsored exam. Needless to say, this is a laughably far cry from a three/four-year Emergency Medicine residency and ABEM board certification for emergency physicians. Can you imagine a nurse practitioner being subject to the oral exam component of the ABEM boards? Not a pretty thought.
Finally, it's also worth touching on the oft-used argument by midlevels, especially those pushing for full practice authority, that their past clinical experience makes their overall level of training comparable, or even superior to (lol) that of physicians. In the case of this particular NP, according to her own LinkedIn profile she worked for 8+ years and almost 6 years, respectively, as an ER nurse and then ICU nurse at Concord Hospital, a decently-sized 295-bed hospital with level 2 trauma accreditation. It's virtually impossible to fathom that a nurse working at such a place for almost 15 years never encountered a patient with something as basic as vaginal discharge. Hell, it would be hard to imagine any emergency physician making it through a single shift without encountering a female patient with some sort of genitourinary complaint. Quantity != quality. After all, medical school is "only" four years in length. And yet, even a second-year or third-year medical student could come up with a differential diagnosis for vaginal discharge, and certainly recognize risk factors for toxic shock syndrome. It is abundantly clear that previous nursing experience and the nurse practitioner educational model is grossly flawed and insufficient. Plain and simple, nursing is not medicine - and it should never be substituted as such.